
EUS-Guided Anastomosis, Drainage, and Vascular Interventions
Pioneering EUS-Guided Anastomosis for Gastric Outlet Obstruction
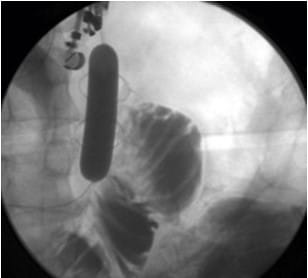
Endoscopic Ultrasonography (EUS)-guided anastomosis marks a significant milestone in the treatment of gastric outlet obstruction. This procedure enables the creation of a connection between the stomach and the jejunum, using a lumen-apposing metal stent (LAMS). The stent placement, which can be achieved directly or with balloon assistance under fluoroscopic and sonographic guidance, showcases the evolving precision in gastrointestinal interventions. Despite the limited experience, early data suggest promising outcomes, offering new hope to patients with this challenging condition.
Advanced Drainage of Abdominopelvic Fluid Collections
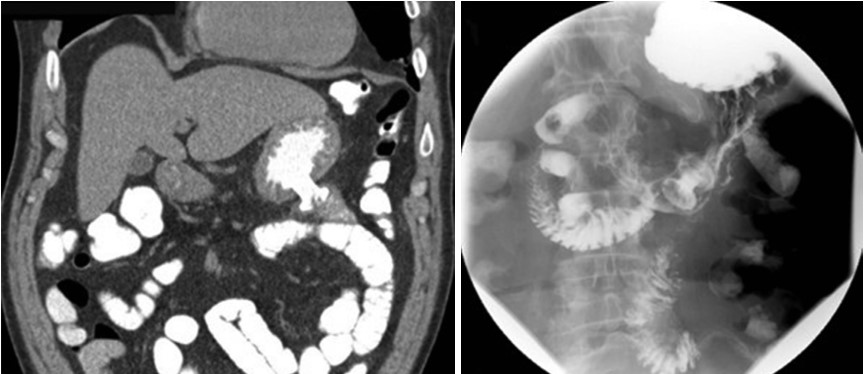
EUS plays a critical role in the transmural drainage of postoperative abdominal and pelvic fluid collections. These collections, located adjacent to the gastrointestinal lumen and within the reach of an echoendoscope, can now be safely and effectively managed. The procedure boasts a high success rate, exceeding 90%, with most adverse events being mild and manageable through conservative means. This advancement underscores the safety and efficacy of EUS-guided interventions in resolving complex postoperative complications.
Essential Tools for Cutting-Edge EUS Procedures
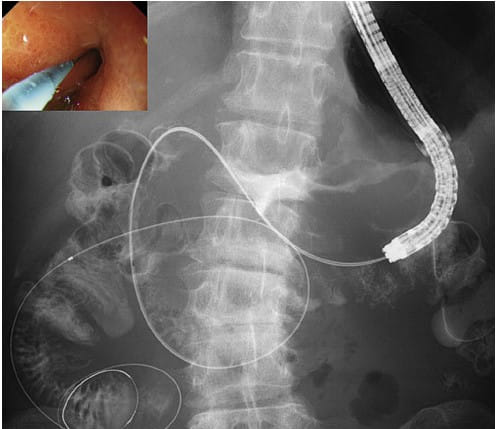
The successful execution of EUS-guided procedures relies heavily on a suite of specialized equipment. This arsenal includes a fluoroscopy unit, a therapeutic echoendoscope, and essential accessories such as 19-G needles, ERCP cannulae, needle-knife catheters, guidewires, balloon dilators, LAMS, double-pigtail plastic stents, and biliary drainage catheters. The availability and proper use of these tools are paramount in performing these advanced interventions, ensuring optimal outcomes for patients.
EUS-Guided Vascular Interventions: A Leap Forward in Hemostasis
EUS-guided hemostasis introduces an innovative approach to managing gastric varices through coil embolization and/or glue injection. This technique has emerged as a clinically effective method for controlling bleeding, demonstrating promising treatment outcomes. The ability to directly visualize and target the treatment area offers a significant advantage over traditional methods, marking a new era in gastroenterological care.
Conclusion
The advent of EUS-guided anastomosis, drainage of abdominopelvic fluid collections, and vascular interventions represents a paradigm shift in gastrointestinal care. These procedures not only provide minimally invasive alternatives to traditional surgical methods but also enhance patient safety and recovery outcomes. As the field of gastroenterology continues to advance, these innovative techniques promise to further improve the quality of life for patients facing complex gastrointestinal challenges.
Disclaimer: This content is for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for personal medical advice.
Learn More About Our Gastroenterology Services
Contact Us for More Information
