Esophageal Diverticula: Causes, Diagnosis, and Treatments
Esophageal diverticula, though relatively rare with a prevalence of up to 3%, are significant when considering esophageal health. They are classified by their cause, location, and wall component. Notably, Zenker diverticula account for 70% of these cases.
What Are Esophageal Diverticula?
Esophageal diverticula are pouches that protrude from the esophageal lining. These can be classified into several types based on their characteristics:
- By Cause:
- Pulsion Diverticula: Caused by increased pressure inside the esophagus.
- Traction Diverticula: Result from inflammation and scarring pulling on the esophagus.
- By Location:
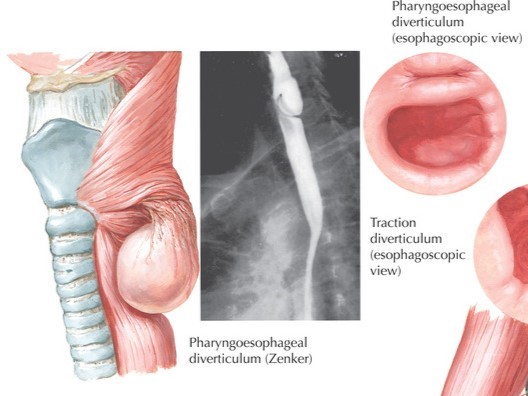
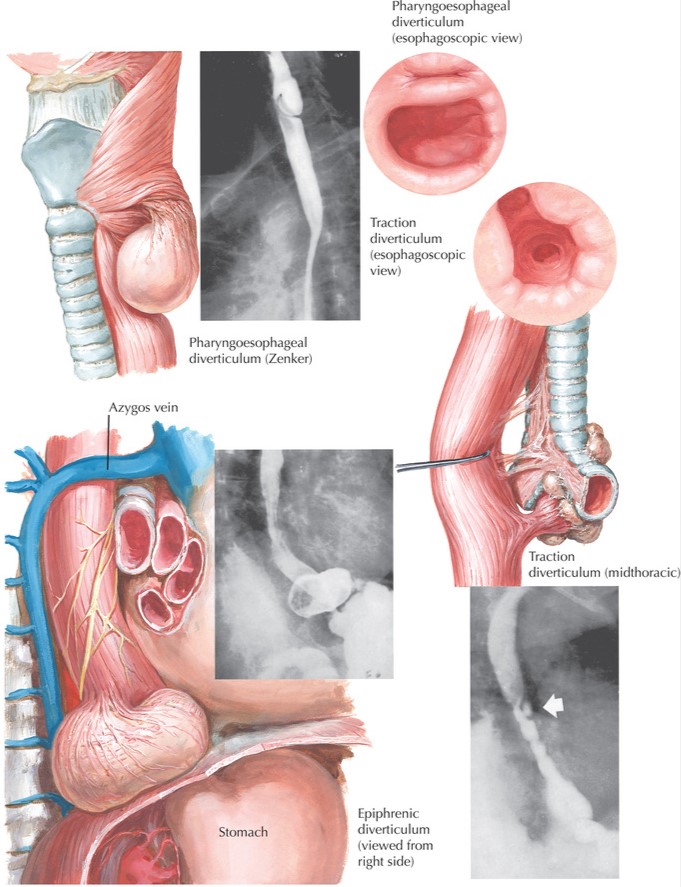
- Pharyngoesophageal (Zenker’s) Diverticula
- Midesophageal Diverticula
- Epiphrenic Diverticula
- By Wall Component:
- True Diverticula: Involve all layers of the esophageal wall.
- Pseudodiverticula: Involve only the mucosal and submucosal layers.
Zenker’s Diverticula: The Most Common Type
Overview
Zenker diverticula are the most prevalent type of esophageal diverticula, occurring more frequently in men around the age of 50. They develop when the mucosa and submucosa herniate through the muscular wall of the hypopharynx, specifically in the Killian triangle.
Symptoms
Early symptoms include a lump sensation in the throat and mucus accumulation. As the condition progresses, patients may experience:
- Foul-tasting food and bad breath (halitosis)
- Dysphagia (difficulty swallowing), initially with liquids, then solids
- Regurgitation of undigested food
- Aspiration pneumonia or lung abscesses in severe cases
- Significant weight loss and malnutrition
Diagnosis
Diagnosis typically involves:
- Physical Examination: Fullness under the left sternocleidomastoid muscle and gurgling on compression.
- Barium Esophagraphy: To determine size and location.
- Esophagoscopy: To visualize the pouch and esophageal structure.
- Manometry: To assess esophageal motility.
Treatment
Surgical intervention is the primary treatment, with options including:
- Open Surgery: Diverticulectomy, invagination, or diverticulopexy with myotomy.
- Endoscopic Surgery: Using rigid or flexible endoscopes to perform diverticulostomy.
Minimally invasive techniques often result in quicker recovery and lower complication rates.
Pulsion Diverticula
Characteristics
These diverticula occur in the distal 10 cm of the esophagus and are often associated with motility disorders like achalasia or diffuse esophageal spasm.
Symptoms
Patients typically present with:
- Dysphagia
- Regurgitation
- Pulmonary symptoms like aspiration
Diagnosis
Diagnosis involves barium esophagraphy, endoscopy, and manometry to identify underlying motility disorders.
Treatment
Surgery is recommended for larger diverticula, with approaches including diverticulectomy and myotomy. Minimally invasive techniques are preferred for their lower morbidity and quicker recovery times.
Traction Diverticula
Causes
These develop due to inflammation and scarring from conditions like tuberculosis or histoplasmosis. They are outpouchings of all esophageal layers.
Symptoms
Most traction diverticula are asymptomatic. When symptoms occur, they include chest pain, odynophagia, and regurgitation.
Diagnosis
Barium swallow and endoscopy can help visualize these diverticula.
Treatment
Surgery is reserved for severe cases and involves thoracotomy to remove the diverticulum without the need for a myotomy.
Conclusion
Esophageal diverticula, while uncommon, can significantly impact quality of life. Early diagnosis and appropriate treatment, particularly surgical intervention for larger or symptomatic diverticula, are crucial. Understanding the different types and their management can help patients and healthcare providers make informed decisions for optimal outcomes.
For more information on esophageal health and treatments, contact us.
