Esophageal Varicosities: Causes, Symptoms, and Treatment
Understanding Esophageal Varicosities: Causes, Symptoms, and Treatment
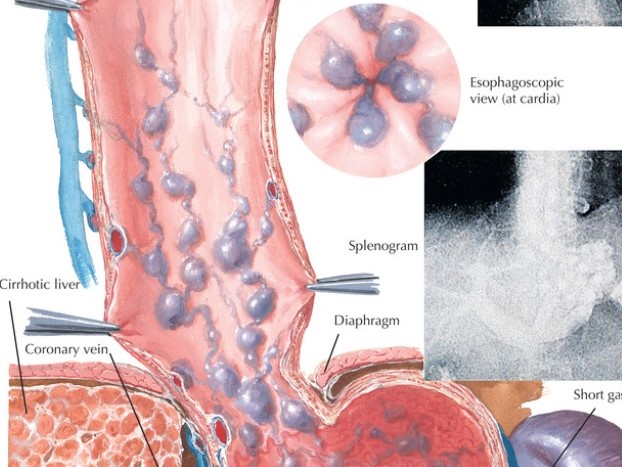
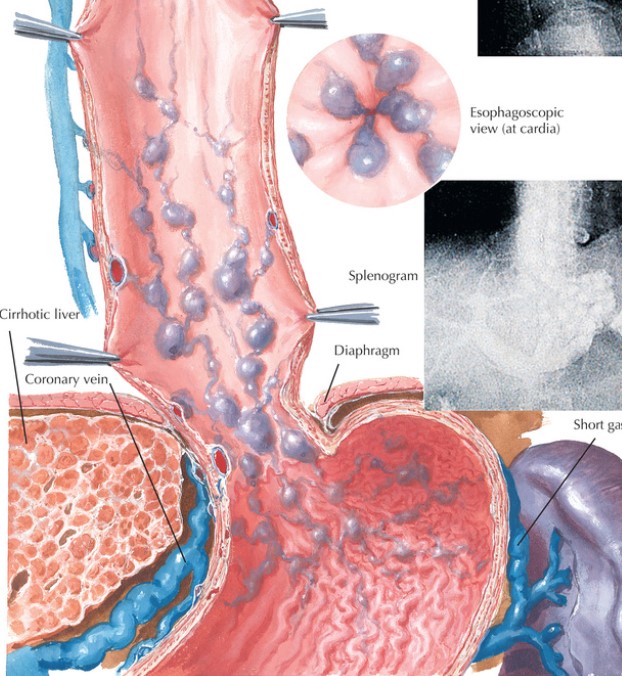
Esophageal varicosities, commonly known as esophageal varices, are dilated veins in the esophagus caused by increased pressure in the portal vein, typically due to liver cirrhosis. These varices are dangerous because they can rupture and cause life-threatening bleeding. This blog provides a comprehensive overview of esophageal varices, including their causes, symptoms, diagnosis, and treatment options.
Causes of Esophageal Varicosities
Esophageal varicosities develop as a result of portal hypertension, which occurs when blood flow through the liver is obstructed due to cirrhosis. The most common causes of cirrhosis include:
- Alcoholism (57%)
- Hepatitis C Virus (30%)
- Hepatitis B Virus (10%)
When the liver is scarred, blood is forced to find alternative pathways, leading to the formation of varices. These varices most often occur in the distal third of the esophagus but can be found throughout the esophagus.
Symptoms of Esophageal Varices
The primary symptoms of esophageal varicosities include:
- Recurrent Hematemesis: Vomiting of blood.
- Melena: Black, tarry stools due to digested blood.
- Hemodynamic Instability: Including symptoms like tachycardia, hypotension, and orthostatic hypotension.
Diagnosis
To prevent a first variceal hemorrhage, patients with cirrhosis should undergo regular screening using upper endoscopy. This procedure helps to detect the presence and severity of varices. Other diagnostic methods include:
- Endoscopic Color Doppler Ultrasonography
- Capsule Endoscopy
- 64-row Multidetector CT Portal Venography
These tools help visualize the varices and assess their hemodynamics, providing critical information for management.
Treatment and Management
Management of esophageal varices involves three phases:
- Prevention of Initial Bleeding: This includes primary prophylaxis with treatments such as nonselective beta-blockers (e.g., nadolol) and endoscopic variceal ligation (EVL).
- Management of Active Bleeding: Acute bleeding requires immediate medical intervention with medications like vasopressin or octreotide and endoscopic treatments such as band ligation or sclerotherapy.
- Prevention of Rebleeding: Secondary prophylaxis involves the use of beta-blockers, EVL, or transjugular intrahepatic portosystemic shunt (TIPS) for high-risk patients.
Prognosis and Follow-Up
The prognosis for patients with esophageal varices depends significantly on liver function. Regular endoscopic surveillance is crucial for early detection and treatment of varices to prevent bleeding. The frequency of endoscopy varies based on the presence and size of varices, and whether the patient has compensated or decompensated cirrhosis.
In summary, esophageal varicosities are a serious complication of liver disease requiring vigilant monitoring and timely treatment. Understanding their causes, symptoms, and management options is essential for preventing life-threatening complications.
For more information on esophageal health and treatment options, contact us
